Metabolic Syndrome: What is it and how to live with it
Introduction To Metabolic Syndrome: Understanding The Cluster Of Conditions
Notice: Always consult your healthcare professional before attempting any of the recommendation in this article.
Metabolic syndrome stands as a multifaceted health challenge, weaving together a tapestry of conditions that, in concert, amplify the risk of heart disease, stroke, and type 2 diabetes. At its core, this syndrome is not identified by a singular symptom or marker but rather by the confluence of several metabolic dysfunctions. These include abdominal obesity—a waistline expanded beyond healthy measures—coupled with elevated blood pressure, increased levels of fasting blood sugar, abnormal cholesterol profiles, and insulin resistance. [Sources: 0, 1, 2]

This constellation of factors does not occur in isolation; they are interlinked in complex ways that exacerbate each other. Understanding metabolic syndrome requires delving into the intricacies of these connections and how they collectively forge a path to more severe health outcomes. [Sources: 3, 4]
The significance of recognizing this syndrome lies not only in identifying the presence of any single condition but in acknowledging the combined impact these conditions have on an individual's overall health. Thus, unraveling the complexities of metabolic syndrome is critical for both prevention and management strategies aimed at mitigating its far-reaching effects on one's well-being. [Sources: 5, 6]
Causes Of Metabolic Syndrome: Genetic And Lifestyle Factors
The interplay between genetic predispositions and lifestyle factors plays a pivotal role in the onset of metabolic syndrome, weaving a complex tapestry that underscores the multifaceted nature of this condition. Genetics lay the groundwork, with certain inherited traits increasing susceptibility to components of metabolic syndrome such as insulin resistance, hypertension, and abnormal lipid profiles. This genetic vulnerability does not act in isolation but interacts dynamically with lifestyle choices and environmental influences. [Sources: 7, 8, 9]

Lifestyle factors serve as catalysts that can either activate these latent genetic predispositions or exacerbate their expression. Poor dietary habits, characterized by excessive intake of high-calorie, nutrient-poor foods, set the stage for obesity and insulin resistance. Physical inactivity compounds this risk by contributing to weight gain and reducing muscle mass, further impairing glucose metabolism. Additionally, chronic stress and inadequate sleep can disrupt hormonal balances essential for maintaining metabolic health. [Sources: 10, 11, 12, 13]
The intricate relationship between genetics and lifestyle choices highlights the complexity of preventing and managing metabolic syndrome. It underscores the importance of adopting a holistic approach that encompasses not only medical interventions but also modifications in diet, physical activity levels, stress management, and sleep hygiene to mitigate this risk effectively. [Sources: 14, 15]

Risk Factors For Metabolic Syndrome: Obesity, Inactivity, And Hormonal Imbalances
The development of metabolic syndrome is closely linked with several risk factors, among which obesity, inactivity, and hormonal imbalances stand out for their significant roles. Obesity, particularly the accumulation of fat around the abdomen, poses a critical risk. This form of central obesity contributes to the resistance of insulin in the body, a hallmark trait of metabolic syndrome. It's not just the presence of excess weight but specifically where this weight is distributed that elevates the risk. [Sources: 16, 17, 18, 19]
Equally important is physical inactivity. A sedentary lifestyle leads to numerous health issues, including an increased chance of developing metabolic syndrome. Regular physical activity helps regulate blood sugar levels, improve blood pressure and cholesterol levels, and maintain a healthy weight—key factors in preventing or managing this condition. [Sources: 3, 11]
Furthermore, hormonal imbalances play a crucial role. Conditions like polycystic ovary syndrome (PCOS), which is marked by insulin resistance alongside other hormonal changes, can elevate the risk for metabolic syndrome. These imbalances can disrupt normal metabolic processes in the body, leading to or exacerbating components of metabolic syndrome. [Sources: 17, 20, 21]

Understanding these risk factors underscores the importance of lifestyle modifications and medical interventions aimed at reducing obesity, increasing physical activity levels, and addressing any underlying hormonal imbalances as strategies for preventing or managing metabolic syndrome effectively. [Sources: 4]
Diagnosis And Monitoring Of Metabolic Syndrome: Identifying The Signs
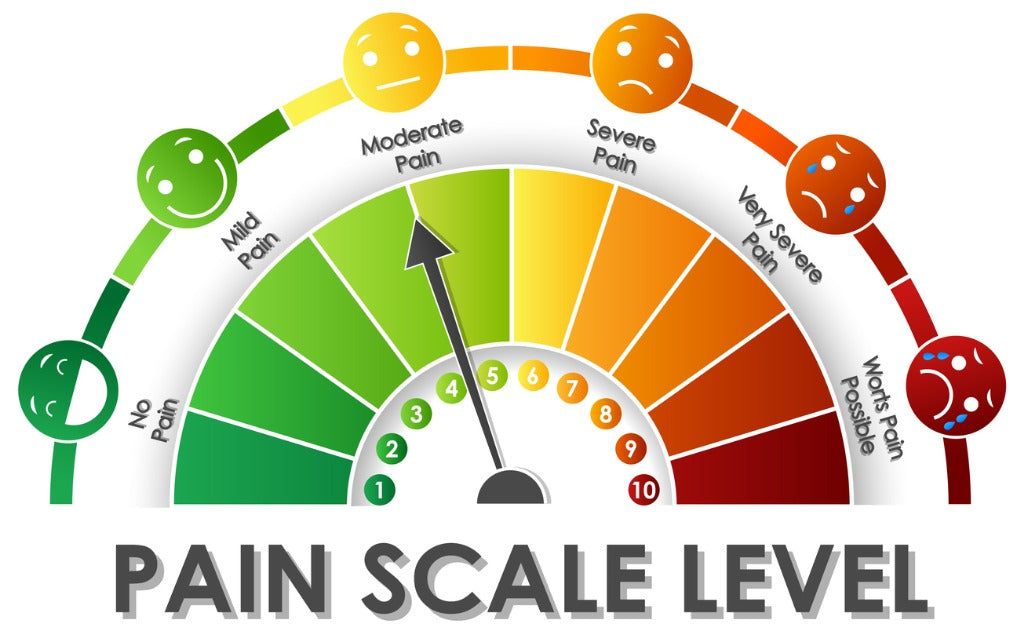
Diagnosing and monitoring metabolic syndrome involves a careful observation of the signs that hallmark this condition, guided by clinical criteria. The process begins with recognizing the constellation of symptoms that are typical for metabolic syndrome. These include central obesity, where fat deposits primarily around the waist, leading to an increased waist circumference—a key indicator. Alongside this, elevated blood pressure readings provide early warning signs, often requiring consistent monitoring to confirm persistent hypertension. [Sources: 1, 4, 22, 23]

Blood tests play a crucial role in uncovering further evidence of metabolic syndrome. Elevated fasting blood sugar levels may indicate insulin resistance or prediabetes, conditions closely linked to the development of metabolic syndrome. Abnormal cholesterol levels, specifically high triglycerides and low high-density lipoprotein (HDL) cholesterol, further contribute to the diagnosis. [Sources: 4, 11]
Monitoring these indicators over time is crucial for managing metabolic syndrome effectively. Regular check-ups allow healthcare providers to track changes in weight, blood pressure, blood sugar, and lipid levels. This ongoing surveillance is essential not only for diagnosing metabolic syndrome but also for evaluating the risk of associated complications such as heart disease and type 2 diabetes. Through vigilant monitoring and early intervention, individuals can significantly reduce their risk and manage their health proactively. [Sources: 24, 25, 26, 27]
Prevention Of Metabolic Syndrome: Strategies For Lowering Your Risk
Preventing metabolic syndrome is pivotal in reducing the risk of heart disease, stroke, and type 2 diabetes. The foundation of prevention lies in adopting a lifestyle that supports overall health and well-being. Central to this approach is maintaining a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. This nutritional strategy helps manage weight and reduces the intake of processed foods high in sugar and saturated fats, which are known contributors to the conditions comprising metabolic syndrome. [Sources: 24, 28, 29, 30]

Regular physical activity is another cornerstone of prevention. Engaging in exercise for at least 30 minutes most days of the week can significantly lower blood pressure, improve cholesterol levels, enhance insulin sensitivity, and support weight management—each an essential factor in mitigating the risk of metabolic syndrome. [Sources: 31, 32]
Additionally, managing stress through mindfulness practices such as meditation or yoga can help control blood pressure and improve overall health. Avoiding smoking and limiting alcohol consumption are also critical since both can exacerbate the conditions associated with metabolic syndrome. [Sources: 33, 34]
By integrating these strategies into daily life, individuals can significantly lower their risk of developing metabolic syndrome. It's about making informed choices each day to support a healthier future. [Sources: 22, 35]
Management Of Metabolic Syndrome: Treatment Options And Medications
Management of metabolic syndrome involves a holistic approach, focusing on lifestyle modifications as the cornerstone of treatment, supplemented by medications when necessary. The primary objective is to reduce the risk of cardiovascular diseases and type 2 diabetes through interventions that address the root causes of the syndrome. [Sources: 36, 37]
Lifestyle changes are paramount and include adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins while minimizing saturated fats, trans fats, and processed foods. Regular physical activity is also crucial; engaging in moderate-intensity exercises for at least 150 minutes a week can significantly improve health markers. Weight loss is encouraged for overweight or obese individuals to reduce abdominal obesity and improve insulin sensitivity. [Sources: 17, 37, 38]

When lifestyle modifications are insufficient to control the conditions associated with metabolic syndrome, medications may be prescribed. Antihypertensive drugs are used to manage high blood pressure, while statins may be recommended for lowering LDL cholesterol levels. For those with high blood sugar levels indicative of prediabetes or diabetes, metformin is often the first-line medication due to its ability to improve insulin sensitivity. [Sources: 11, 39, 40]
Ultimately, managing metabolic syndrome requires a committed partnership between individuals and their healthcare providers to tailor a plan that addresses specific health needs and risks effectively. [Sources: 41]
Lifestyle Changes For Metabolic Syndrome: The Importance Of Diet And Exercise
Lifestyle changes, particularly in diet and exercise, are pivotal in managing metabolic syndrome and mitigating its associated risks. A nuanced understanding of these lifestyle modifications can illuminate the path to better health. Diet plays a crucial role; it's not solely about reducing caloric intake but focusing on the quality of food consumed. Incorporating a diet rich in fruits, vegetables, whole grains, and lean proteins while minimizing processed foods, sugars, and saturated fats can significantly impact one’s metabolic profile. [Sources: 42, 43, 44]
This dietary shift aims to reduce abdominal obesity - a key player in metabolic syndrome - improve insulin sensitivity, and normalize blood pressure and lipid levels. [Sources: 45]
Parallel to dietary adjustments is the importance of regular physical activity. Exercise acts as a powerful tool in combating metabolic syndrome by enhancing weight loss, improving insulin resistance, and bolstering cardiovascular health. Engaging in moderate-intensity activities such as brisk walking or cycling for at least 150 minutes per week is recommended. This combination of dietary changes and consistent physical activity creates a synergistic effect that not only addresses the components of metabolic syndrome but also fosters overall well-being. [Sources: 12, 22, 32, 33]
Weight Management In Metabolic Syndrome: Controlling Abdominal Obesity
Weight management plays a pivotal role in controlling abdominal obesity, a key component of metabolic syndrome. At its core, managing weight to combat abdominal obesity involves a comprehensive approach that includes dietary modifications, increased physical activity, and behavioral changes. A diet rich in fruits, vegetables, whole grains, and lean proteins can significantly reduce caloric intake while providing essential nutrients. This nutritional strategy not only aids in weight loss but also improves overall metabolic health. [Sources: 17, 32, 46, 47]
Increasing physical activity is equally crucial. Engaging in regular exercise such as walking, cycling, or swimming for at least 150 minutes per week can help burn excess calories and reduce abdominal fat. Moreover, physical activity enhances insulin sensitivity and cardiovascular health. [Sources: 24, 48, 49]
Behavioral changes focusing on lifestyle modifications are fundamental to sustaining weight loss and preventing regaining of abdominal fat. Strategies such as setting realistic goals, keeping a food diary, and seeking support from friends or professionals can motivate individuals to adhere to their weight management plan. [Sources: 50, 51]
Together, these strategies aimed at weight management address the root cause of abdominal obesity within the context of metabolic syndrome. Successfully managing weight not only diminishes the risk associated with metabolic syndrome but also fosters long-term health benefits beyond the immediate goal of reducing waist circumference. [Sources: 39, 52]
Blood Sugar Control In Metabolic Syndrome: Regulating Insulin Levels
Blood sugar control is a pivotal aspect of managing metabolic syndrome, primarily because it revolves around regulating insulin levels within the body. Insulin, a hormone produced by the pancreas, plays a crucial role in how the body uses and stores glucose and fat. In individuals with metabolic syndrome, insulin resistance often occurs, where cells in muscles, fat, and the liver start responding poorly to insulin and cannot easily take up glucose from the blood. [Sources: 41, 53, 54]

As a result, the pancreas produces more insulin to help glucose enter cells. This excess insulin in the bloodstream can lead to various health issues including type 2 diabetes. [Sources: 33, 55]
Addressing blood sugar control involves a multifaceted approach. It includes lifestyle modifications such as adopting a healthy diet rich in fruits, vegetables, whole grains, and lean proteins while minimizing refined sugars and saturated fats. Regular physical activity also enhances the muscle's ability to use insulin and absorb glucose. In some cases, medication might be necessary to help manage blood sugar levels effectively. [Sources: 11, 56, 57, 58]
These strategies collectively aim at improving insulin sensitivity and achieving better overall blood sugar control as part of managing or preventing metabolic syndrome. [Sources: 4]
Stress Management In Metabolic Syndrome: Taking A Holistic Approach To Health
Stress management plays a pivotal role in addressing metabolic syndrome, advocating for a holistic approach to health that transcends mere dietary and exercise adjustments. Chronic stress, by triggering the body's fight-or-flight response, exacerbates metabolic syndrome's characteristics through increased cortisol levels. This hormonal surge can lead to insulin resistance, abdominal obesity, and elevated blood pressure—key components of metabolic syndrome.[Sources: 4, 59, 60]

Incorporating stress reduction techniques into one’s lifestyle is not just beneficial but essential. Mindfulness practices, such as meditation and deep-breathing exercises, have shown promise in lowering cortisol levels, thereby indirectly mitigating the risk factors associated with metabolic syndrome. Similarly, engaging in regular physical activity not only improves cardiovascular health and assists in weight management but also serves as an effective stress reliever. [Sources: 35, 61, 62]
Moreover, fostering strong social connections and seeking professional counseling when necessary can provide emotional support that buffers against life’s stresses. Adopting a holistic approach that includes stress management alongside traditional interventions targets the intricate web of factors contributing to metabolic syndrome. It underscores the importance of treating the individual as a whole—mind, body, and spirit—in pursuit of optimal health. [Sources: 4, 63]
Sources
[0]: https://www.medichecks.com/blogs/longevity/what-is-metabolic-syndrome-and-can-you-prevent-it
[1]: https://rosewellness.com/insulin-resistance-and-metabolic-syndrome/
[2]: https://www.yourhormones.info/endocrine-conditions/metabolic-syndrome/
[3]: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/metabolic-syndrome
[4]: https://casadesante.com/blogs/gut-health/a-functional-medicine-treatment-protocol-for-metabolic-syndrome-testing-nutrition-and-supplements
[5]: https://healthify.nz/health-a-z/m/metabolic-syndrome/
[6]: https://rhealthc.com/conditions/metabolic-disorders/
[7]: https://news.osu.edu/stress-via-inflammation-is-linked-to-metabolic-syndrome/
[8]: https://www.bvhealthsystem.org/expert-health-articles/what-is-insulin-resistance-what-is-metabolic-syndrome
[9]: https://academic.oup.com/toxsci/article/162/1/36/4585010
[10]: https://www.racgp.org.au/afp/2013/august/the-metabolic-syndrome
[11]: https://thekingsleyclinic.com/metabolic-syndrome-explained-symptoms-diagnosis-treatment-self-care/
[12]: https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2023.1253506/full
[13]: https://ezra.com/blog/metabolic-health
[14]: https://www.yourhealth.net.au/articles/lifestyle/managing-metabolic-syndrome-with-lifestyle-changes/
[15]: https://hsrc.himmelfarb.gwu.edu/smhs_crl_facpubs/427/
[16]: https://www.abcam.com/content/metabolic-syndrome-mechanisms-pathophysiology-and-laboratory-assessment
[17]: https://www.linkedin.com/pulse/metabolic-syndrome-rise-insights-understanding-management-r-anavf
[18]: https://aviishaaya.com/blog/understanding-metabolic-syndrome-and-how-it-affects-the-body
[19]: https://www.mayoclinic.org/diseases-conditions/obesity/multimedia/vid-20536756
[20]: https://www.nbcnews.com/health/health-news/ozempic-other-health-conditions-pcos-alzheimers-rcna90457
[21]: https://www.rupahealth.com/post/a-functional-medicine-treatment-protocol-for-metabolic-syndrome-testing-nutrition-and-supplements
[22]: https://wildirismedicaleducation.com/courses/metabolic-syndrome-ceu
[23]: https://draxe.com/health/metabolic-syndrome/
[24]: https://crossfittorque.com/metabolic-syndrome-101-with-a-nutrition-coach/
[25]: https://appledoremedicalgroup.com/blog/entry/metabolic-syndrome-101
[26]: https://www.rupahealth.com/post/how-to-test-your-patients-for-metabolic-syndrome-a-functional-medicie-approach
[27]: https://weightmatters.co.uk/2019/07/30/lifestyle-medicine-changing-way-manage-health/
[28]: https://www.cardiosmart.org/topics/metabolic-syndrome/living-with-metabolic-syndrome
[29]: https://www.queens.org/metabolic-syndrome-causes-prevention/
[30]: https://www.healthifyme.com/blog/metabolic-syndrome/
[31]: http://journals.seedmedicalpublishers.com/index.php/rhc/article/view/667/1015
[32]: https://www.healthywomen.org/condition/metabolic-syndrome
[33]: https://www.freemanmedicalclinic.com/post/metabolic-syndrome-and-insulin-resistance
[34]: https://www.signos.com/blog/metabolic-syndrome-diet
[35]: https://cura4u.com/blog/link-between-obesity-and-chronic-health-conditions
[36]: https://www.nhs.uk/conditions/metabolic-syndrome/
[37]: https://drwaseemclinic.com/insulin-resistance-in-metabolic-syndrome/
[38]: https://www.oecd-ilibrary.org/sites/561b552e-en/index.html?itemId=/content/component/561b552e-en
[39]: https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-metabolic-syndrome-and-lifestyle-changes/
[40]: https://www.medicinenet.com/metabolic_syndrome/article.htm
[41]: https://www.janahealthcare.com/blog/decoding-insulin-resistance-understanding-its-role-in-weight-gain-and-the-path-to-healthy-weight-ma
[42]: https://joymedical.com/metabolic-syndrome-understanding-the-cluster-of-conditions-and-how-to-manage-it/
[43]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1783583/
[44]: https://diabetesjournals.org/care/article/28/12/2823/22802/Beneficial-Effects-of-a-Dietary-Approaches-to-Stop
[45]: https://www.texasheart.org/heart-health/heart-information-center/topics/metabolic-syndrome/
[46]: https://www.rupahealth.com/post/cardiovascular-disease-and-metabolic-syndrome-addressing-root-causes-with-functional-medicine
[47]: https://www.kidney.org/atoz/content/obesity
[48]: https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2022.809669/full
[49]: https://www.jomes.org/journal/view.html?doi=10.7570/jomes21022
[50]: https://www.endocrinewellness.com/weight-management/
[51]: https://www.nhs.uk/conditions/obesity/
[52]: https://www.news-medical.net/news/20230210/Can-lifestyle-and-nutrition-be-the-answer-for-metabolic-syndrome-and-type-2-diabetes-remission.aspx
[53]: https://medlineplus.gov/genetics/condition/type-a-insulin-resistance-syndrome/
[54]: https://www.kitsapchiro.com/metabolic-syndrome/
[55]: https://thevitalityclinic.co.uk/personality-trait-and-genetic-variants-and-the-metabolic-syndrome/
[56]: https://www.heartuk.org.uk/genetic-conditions/metabolic-syndrome
[57]: https://www.hilarispublisher.com/open-access/abdominal-obesity-and-metabolic-syndrome-101972.html
[58]: https://www.ncbi.nlm.nih.gov/books/NBK507839/
[59]: https://www.signos.com/blog/hormones-metabolic-syndrome
[60]: https://www.medicinenet.com/insulin_resistance/article.htm
[61]: https://www.awakenedpathcounseling.com/holistic-guide-to-managing-stress/
[62]: https://dhwblog.dukehealth.org/holistic-approaches-to-managing-diabetes/
[63]: https://www.vitrywellness.com/blogs/blog/1170514-holistic-approaches-to-stress-management